Cooling of Obese Patients
Robert B. Schock, Ph.D.
From the Department of Research and Development, The Sid Wolvek Research Center, Life Recovery Systems HD LLC, Kinnelon, NJ USA
Obesity is a medical challenge that has grown to epidemic proportions in the United States. As of 2007, 26% of Americans were classified as being obese, having a body mass index (BMI) of 30 or more.1 Obese patients are at a significantly higher risk of suffering heart attacks, cardiac arrests, and strokes compared to patients of normal weight. Given this, a high proportion of patients requiring therapeutic hypothermia are obese.
Larger patients present a particular challenge for cooling as they contain more heat, and their higher body mass relative to surface area reduces the efficacy of surface cooling. A multi-center study of cooling blankets and the Medivance Arctic Sun reported typical cooling times of 3 to 4 hours, but this was for patients below 250 lbs.2 A second study of the Arctic Sun observed a trend for slower cooling rates for larger patients, and found that some patients required as much as 8 hours to reach target temperatures.3 The authors noted, “…patients with very high BMI (>35) tended to cool slowly.
A similar challenge exists for cooling catheters; in a recent study4 it was noted that “larger patients are more difficult to cool and maintain in therapeutic rangeâ€. In some cases it was impossible to achieve or maintain therapeutic hypothermia with these devices.†The study concluded, “…the most important variable in successfully initiation and maintaining therapeutic hypothermia was weight, and specifically the body surface area.â€
Two new studies related to this topic were recently presented at the 2012 RESS meeting. One was a five-year study of conventional external surface cooling5 which found that obesity extended cooling times by an average of 67 minutes (p=0.07). The study also found that “Obese patients were significantly more likely to experience skin breakdown as a result of therapeutic hypothermiaâ€. A second institution reported results of a three-year study6 in which obese patients represented 55% of the patients that required therapeutic hypothermia. Obese patients required 78 minutes more cooling time to reach target temperatures than non-obese patients (p=0.012). The authors concluded, “obese patients potentially represent a population where additional approaches may be needed to improve cooling times.â€
One such additional approach is the LRS ThermoSuit System7, 8, which can provide the most rapid patient cooling of any noninvasive device. This has a particular advantage in cooling of large patients. A multicenter clinical trial of the ThermoSuit System9 found that non-obese patients required an average cooling time of 38.3 minutes, and obese patients cooled in an average of 47.5 minutes. These results are clearly superior to those observed with conventional surface cooling, as can be seen in the chart below:
Patient Cooling Times (minutes to 34°C)
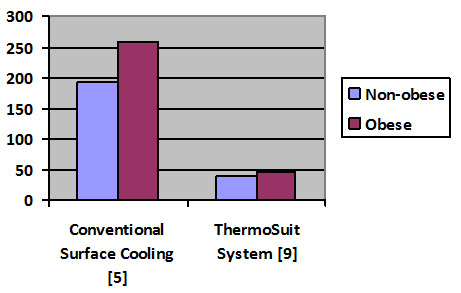
The above chart shows that the ThermoSuit cooling method provides a faster cooling rate compared to conventional surface cooling for both non-obese patients (BMI < 30) and obese patients (BMI ≥ 30).
The ice water immersion technique as used by the Thermosuit is capable of extracting heat approximately five times as rapidly as conventional surface cooling.10 The ThermoSuit applies liquid convection cooling to nearly all of the body surface area, while conventional cooling blankets and the Medivance Arctic Sun gel pads contact a relatively small portion of the patient. The combination of a high surface area of cooling with a high rate of heat extraction per unit of surface area produces the class-leading cooling rate for patients treated with the ThermoSuit.

ThermoSuit System cooling high-BMI patient.
[1] U.S. National Health and Nutrition Examination Survey, 2007
[2] Heard KJ et al, “A randomized controlled trial comparing the Arctic Sun to standard cooling for induction of hypothermia after cardiac arrestâ€, Resuscitation 2010 Vol 81, No. 1, 9-14.
[3] Jarrah S et al, “Surface Cooling after Cardiac Arrest: Effectiveness, Skin Safety, and Adverse Events in Routine Clinical Practiceâ€, Neurocrit Care 2011; 14: 382-388.
[4] Lyden P et al, “Determinants of Effective Cooling during Endovascular Hypothermiaâ€, Neurocrit Care 2012 June; 15(3): 413-420.
[5] Leary M et al, “Association of Body Mass Index with Time to Target Temperature and Outcomes in Postarrest Patients Treated with Therapeutic Hypothermia via an External Cooling Systemâ€, Abstract 210, Resuscitation Science Symposium, AHA 2012.
[6] Schauer J, Kupas D, “Obesity and Cooling Time to Target Temperature in Patients Undergoing Therapeutic Hypothermia after Out-of-Hospital Cardiac Arrestâ€, Abstract 151, Resuscitation Science Symposium, AHA 2012.
[7] Howes D, Ohley W, Dorian P, Klock JC, Freedman R, Schock R, Krizanac D, Holzer M, “Rapid Induction of Therapeutic Hypothermia using Convective-Immersion Surface Cooling: Safety, Efficacy, and Outcomesâ€, Resuscitation 2010 Vol. 81, no .4, 388-392.
[8] Kudagi VS, McMullan PW, Jr., White CJ, “Rapid induction of therapeutic hypothermia in comatose survivors of cardiac arrest using liquid-convection immersion cooling”, Society for Cardiovascular Angiography and Interventions 2012 (Abstract).
[9] Howes D et al, ThermoSuit Clinical Trial NCT00410969, overall results published in Resuscitation 2010.
[10] Plattner O et al, ” Efficacy of Intraoperative Cooling Methods”, Anesthesiology 1997 87(5):1089-1095.


